Understanding Obsessive Compulsive Disorder (OCD)
The complicated mental illness known as obsessive-compulsive disorder (OCD) is typified by recurrent, bothersome thoughts (called obsessions) and repetitive actions or thoughts (called compulsions).
Millions of people are impacted globally, which lowers their quality of life and daily functioning. An extensive examination of OCD’s symptoms, causes, diagnosis, available treatments, and coping mechanisms is given in this article.
1. Is Obsessive-Compulsive Disorder defined?

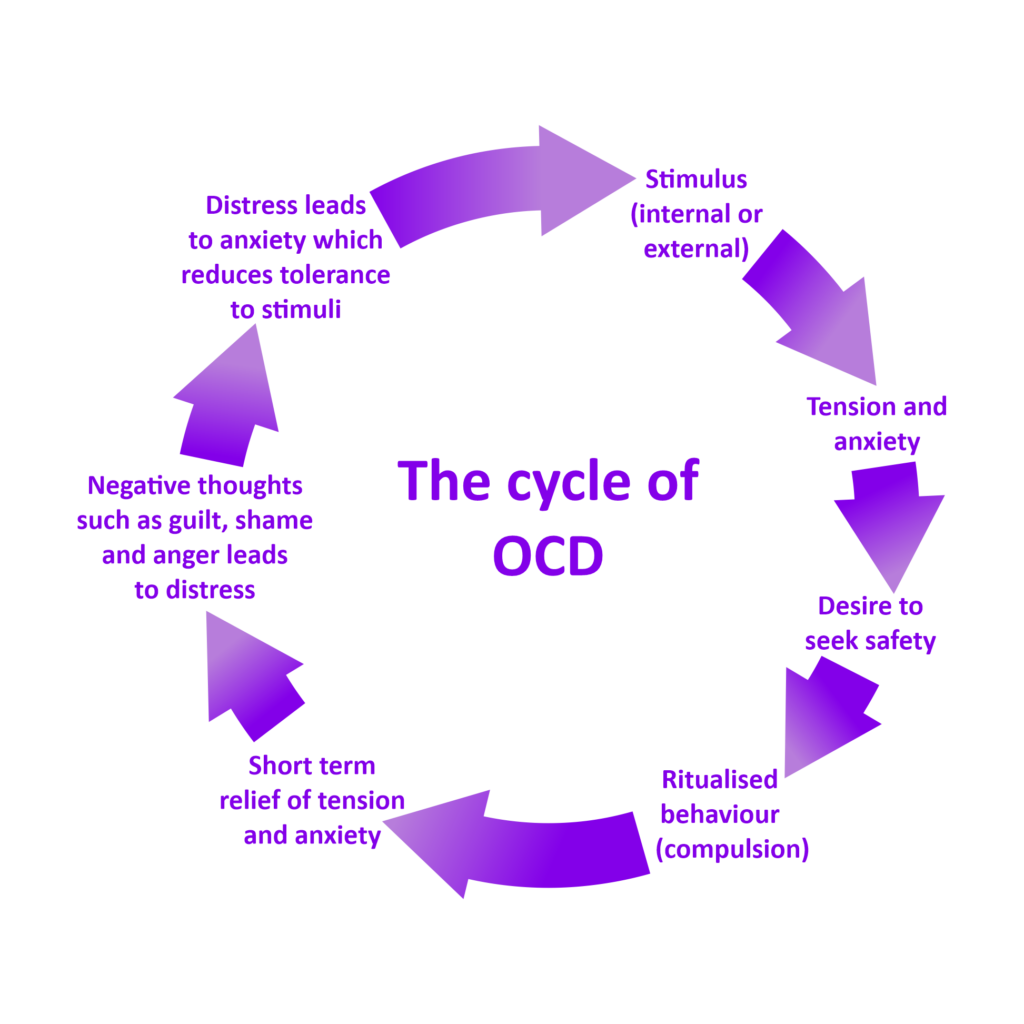
An ongoing cycle of obsessions and compulsions characterises obsessive-compulsive disorder.
Unwanted and upsetting ideas, pictures, or cravings that recur frequently in a person’s thoughts are known as obsessions.
Repetitive actions or thoughts carried out as a means of preventing an event or circumstance that causes anxiety are known as compulsions.
Even after carrying out these routines, OCD sufferers frequently discover that their anxiety either returns or endures, starting a vicious cycle that can be challenging to overcome.
2. OCD symptoms
Although OCD symptoms might differ greatly from person to person, they often fall into two groups:
2.1. Fixations
An individual with an obsession is unable to dismiss thoughts or urges that are bothersome and obtrusive. Typical fixations consist of:
Fear of contamination: A fear of dirt, poisons, or microbes.
Fear of hurting other people: Anxiety over unintentionally hurting people or acting violently.
Fear of committing an error: fear of making mistakes or neglecting anything crucial when completing duties.
Thoughts that are sexual or aggressive: Unsettling ideas of inappropriate or violent behaviour.
Need for symmetry: An intense need for symmetry or order in the world.
2.2. Needs
Compulsions are actions taken, either mentally or physically, to lessen the anxiety brought on by obsessions.
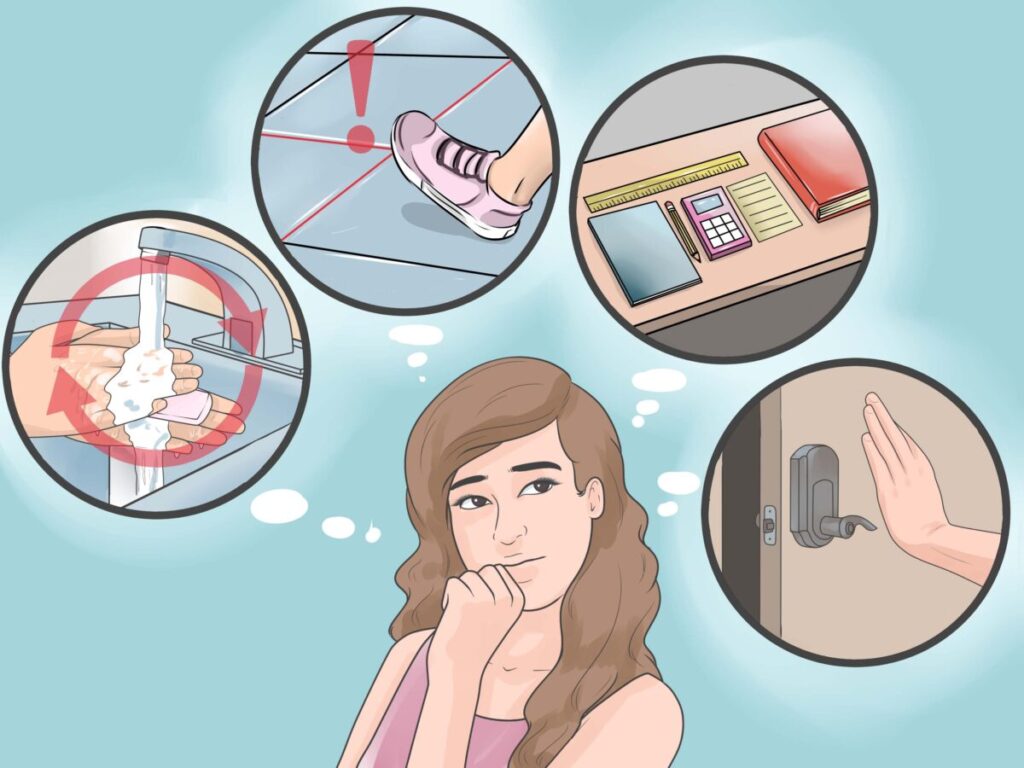
Typical compulsives include: Hand washing and surface cleaning: To lessen the worry of contamination, do these tasks frequently.
Checking: Making sure everything is safe and working correctly by routinely checking locks, appliances, and other items.Counting is the practice of repeatedly counting things or activities to stop a feared outcome.
Sorting and arranging: Putting things in a certain sequence to create symmetry or order.
Mental rituals: Counting or praying in your head to calm yourself down.
3. OCD Causes
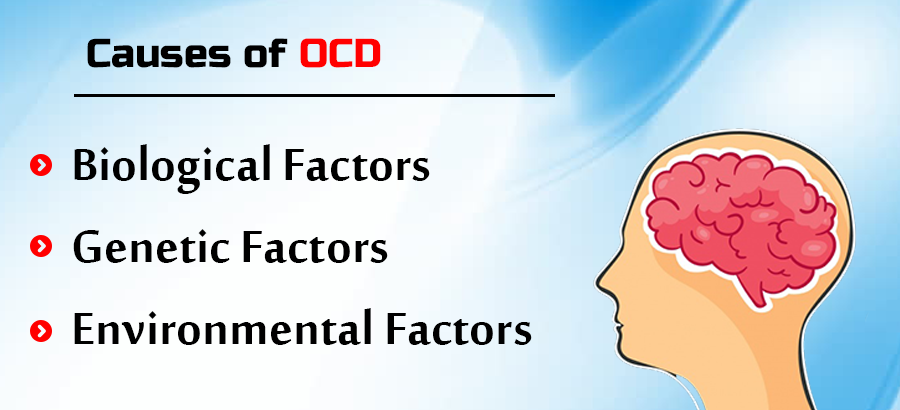
Although the precise aetiology of obsessive compulsive disorder is unknown, evidence points to a potential genetic, biochemical, and environmental component combination.
3.1. Hereditary Elements
obsessive compulsive disorder can run in families, according to family studies, which suggests a hereditary susceptibility. Although no single gene has been found to be the cause of OCD, some genes may impact a person’s vulnerability to the disorder.
3.2. Biochemical Elements
Brain anatomical and functional abnormalities are indicated by neurobiological studies. Neurotransmitter imbalances, specifically in serotonin, could be involved. According to research on brain imaging, individuals with obsessive compulsive disorder frequently have increased activity in certain areas of the brain, including the caudate nucleus, anterior cingulate cortex, and orbitofrontal cortex.
3.3. Elements of the Environment
OCD symptoms can be brought on by or made worse by traumatic or stressful life experiences, such as abuse, grief, or significant life transitions. In many situations, especially involving children, infections and diseases have also been connected to the emergence of OCD through a disorder called Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS).
4. OCD diagnosis

A thorough assessment conducted by a mental health expert is necessary to diagnose obsessive compulsive disorder. Usually, the evaluation consists of:
Clinical Interview: During this conversation, the patient’s symptoms, duration, and daily impact will be discussed with the clinician.
Diagnostic Standards: The Diagnostic and Statistical Manual of Mental Disorders’ (DSM-5) standards serve as the foundation for the diagnosis. OCD is diagnosed, as the DSM-5, when obsessions and/or compulsions are severe, causing more than an hour’s worth of distress or impairment per day.
Instruments for Assessment: The degree of symptoms can be evaluated using standardised rating scales and questionnaires, including the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).
5. Obsessive compulsive disorder Treatment Options
Treatment for obsessive compulsive disorder that works often combines medication, therapy, and self-help techniques.
Cognitive-Behavioral Therapy (CBT): A Review
When it comes to treating OCD, CBT—specifically, Exposure and Response Prevention, or ERP—is regarded as the best approach. ERP entails exposing the person to the things or circumstances they are afraid of while supporting them in abstaining from obsessive actions. This procedure eventually lessens the tension brought on by obsessions and aids in ending the vicious cycle of compulsions.
5.2. Drugs
SSRIs, or selective serotonin reuptake inhibitors, are frequently administered to treat obsessive compulsive disorder symptoms. It has been discovered that drugs including paroxetine, fluoxetine, fluvoxamine, and sertraline are useful in symptom reduction. It’s critical that people collaborate closely with their healthcare professional to select the appropriate drug and dosage
5.3. Alternative Treatments
Some people might benefit from additional therapies: Instead of attempting to control people’s ideas and feelings, acceptance and commitment therapy (ACT) focusses on assisting them in accepting them.
Mindfulness-Based Cognitive Therapy (MBCT): This approach helps people control their thoughts and emotions by fusing cognitive therapy with mindfulness techniques.
5.4. Techniques for Self-Help
For obsessive compulsive disorder sufferers, self-help techniques might be just as important as medical care.
Support Groups: Making connections with other OCD sufferers can be a great way to get advice and support.
Mindfulness and Relaxation Techniques: Stress and anxiety can be effectively managed with the aid of techniques like yoga, meditation, and deep breathing.
Education: Gaining knowledge about OCD can empower people and lessen their sense of loneliness.
6. Having OCD

Although having OCD can be difficult, with the right care and assistance, people can enjoy happy, fulfilled lives. It’s critical that OCD sufferers understand that:
Recovery is Possible: With treatment, a lot of OCD sufferers see notable improvements in their quality of life.Assistance and encouragement can be obtained from mental health specialists, support groups, and educational resources.
Self-Care Matters: Putting self-care first, controlling stress, and reaching out to others for help can all improve general wellbeing.
Is meditation can help recovering from OCD

While it’s not usually thought of as a stand-alone treatment for Obsessive-Compulsive Disorder (OCD), meditation can be a useful part of a more comprehensive treatment strategy.
There are a number of advantages to meditation, particularly mindfulness meditation, which may aid in the healing process.
Summary
Obsessive-Compulsive Disorder is a complex illness that has a significant impact on people. OCD sufferers and those close to them can better manage the disorder’s problems if they are aware of its symptoms, causes, and available treatments.
People with OCD can work towards controlling their symptoms and enhancing their quality of life with a combination of professional therapy, self-help techniques, and support.
A mental health professional’s assistance is essential if you or someone you know is experiencing OCD symptoms. This can help you recover and lead a more balanced, healthy life.



